Acne is one of the most common skin conditions, especially in adolescents, although it can also appear in adulthood. Although we tend to associate it with ‘oily skin’, hormones or stress, the reality is that acne is a multifactorial condition: hormonal, genetic, environmental and inflammatory factors, lifestyle and even gut microbiota all play a role.
In recent years, scientific evidence has shown that diet can directly influence the onset, severity and progression of acne. In this article, we explain in simple terms how acne occurs, why certain foods make it worse and what nutritional changes can really help improve your skin.
What is acne vulgaris?
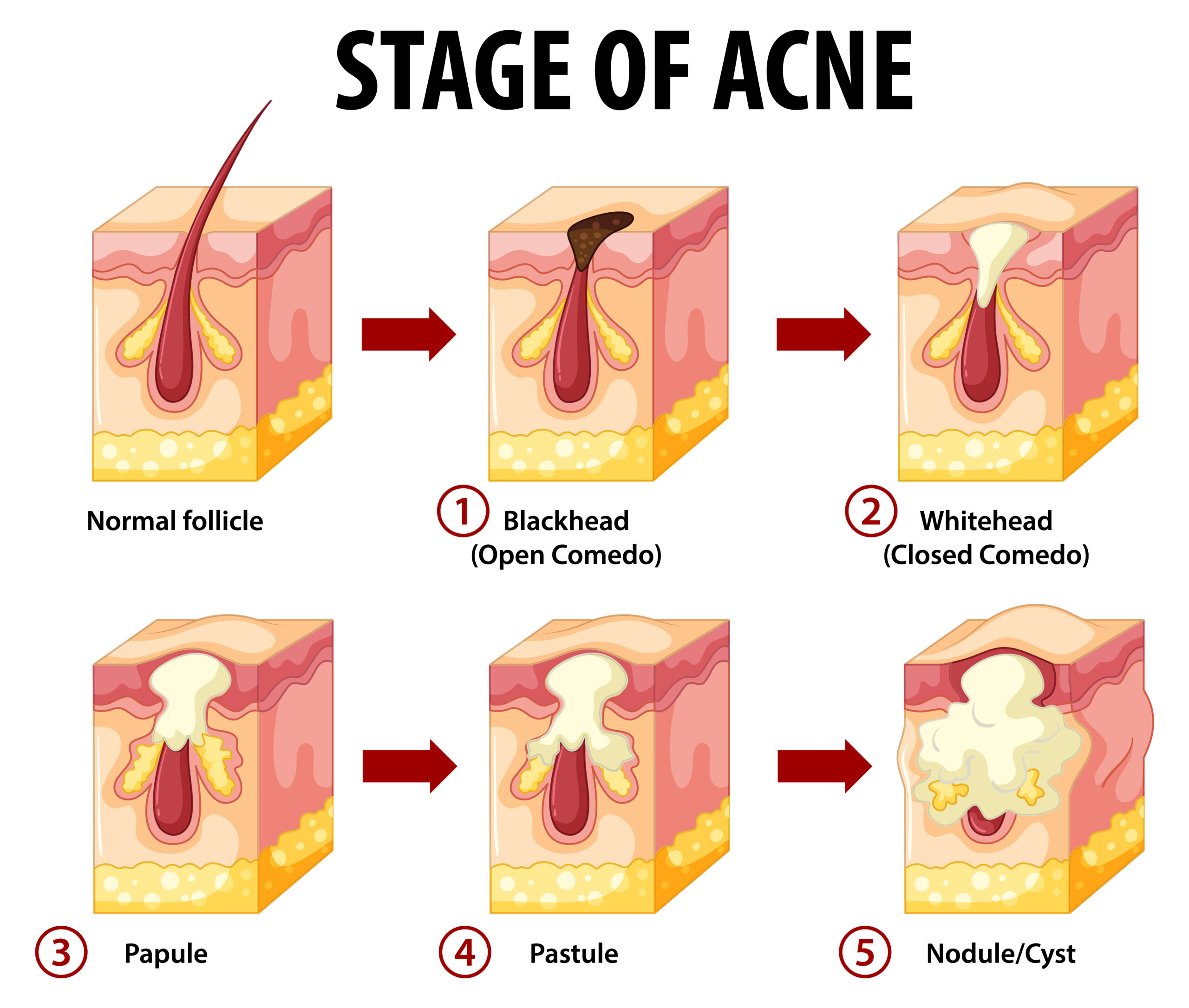
Acne vulgaris is a disease of the pilosebaceous unit. It occurs when the follicle becomes blocked by sebum, keratin and bacteria, causing lesions such as:
- Closed comedones (whiteheads)
- Open comedones (blackheads)
- Papules (inflamed and painful bumps)
- Pustules (with pus)
- Nodules (deep and hard)
- Cysts (inflammatory, painful and with thick content)
- Scars
It is a disease that occurs in outbreaks and has a strong inflammatory component.
How does acne form? The pathophysiology behind the lesions
Several processes occur simultaneously:
1. Sebaceous hypersecretion
Excess sebum is influenced by androgenic hormones, insulin, and an increase in IGF-1. The latter inhibits the FoxO1 factor and activates the mTORC1 pathway, which stimulates sebum production and cell proliferation in the skin.
2. Follicle obstruction
Hyperproliferation of keratinocytes and their adhesion block the sebum outlet.
3. Proliferation of Cutibacterium acnes
The lack of oxygen inside the blocked follicle and the abundance of sebum encourage the bacteria to multiply.
4. Inflammation
Oxidised sebum, free fatty acids and the immune response amplify inflammation, causing more painful and persistent lesions.
Hormones and acne: the connection we cannot ignore
The key hormones in acne are:
- Androgens: increase the size of the sebaceous gland and sebum production.
- Insulin and IGF-1: enhance cell proliferation, lipid synthesis and the conversion of testosterone to its most active form (DHT).
- CRH and melanocortins: released in stressful situations, they aggravate inflammation.
In addition, there are hormonal stages or situations that increase the risk of acne:
Polycystic ovary syndrome (PCOS)
Closely related to insulin resistance and hyperandrogenism.
Adult, perimenopausal and menopausal acne
The drop in oestrogen, insulin resistance and the relative predominance of androgens favour outbreaks.
The role of diet in acne
Diet influences acne because it can:
- Increase or reduce inflammation
- Alter the gut microbiota
- Modify hormone production
- Affect insulin and IGF-1 levels
Population studies have shown that non-Westernised societies have virtually no acne… until they adopt a diet rich in ultra-processed foods, dairy products and sugars.
Foods and habits that worsen acne
1. High glycaemic index diets
Foods that rapidly raise blood sugar increase insulin and IGF-1, promoting:
- More sebum
- More free androgens
- More keratinocyte proliferation
- Worse inflammation
These include: white bread, pastries, sugary cereals, soft drinks, potatoes, white rice, refined pasta.
2. Unfermented dairy products (especially skimmed)
Milk:
- Increases insulin (even with a low GI)
- Provides IGF-1
- Activates mTORC1
- Contains proteins (casein and whey) that trigger insulin
Skimmed milk shows a greater link to acne than whole milk.
3. Excess saturated and trans fats
A diet rich in omega-6 and low in omega-3 promotes an inflammatory environment in the skin.
4. Milk chocolate or sugar
The problem is not cocoa, but:
- sugar
- milk
- added fats
Dark chocolate with a high percentage of cocoa does not show this effect.
5. Excess leucine and glutamine
Found in whey protein supplements and large amounts of meat → activate mTORC1.
6. Alcohol
Increases testosterone, worsens the microbiota and can promote bacterial growth on the skin.
Foods and nutrients that improve acne
1. Omega-3
They are anti-inflammatory, reduce IGF-1 and regulate sebum production.
Oily fish, flax seeds, chia seeds, walnuts.
2. Essential vitamins
Vitamin A: regenerative and antioxidant
Vitamin C: healing and antioxidant
Vitamin D: low in patients with acne; reduces sebum and C. acnes
Vitamin E: antioxidant and anti-inflammatory
B vitamins: regulate sebaceous secretion (except B12 in excess)
3. Minerals
- Zinc: bacteriostatic and anti-inflammatory
- Selenium: regulates sebum and reduces oxidative stress
4. Green tea
The compound EGCG inhibits mTORC1 and SREBP-1, decreasing sebum production.
5. Probiotics
Restore microbiota, regulate glucose, reduce free androgens and increase SHBG. Lactobacillus acidophilus and L. rhamnosus are particularly useful.
6. Antioxidant foods
The Mediterranean diet is the richest in this group: fruits, vegetables, legumes, EVOO, seeds, nuts, oily fish.
Nutritional strategies that help improve acne
1. Low glycaemic index diet
Reduces:
- size of sebaceous glands
- sebum production
- inflammatory lesions
- SREBP-1
This is one of the most effective interventions.
2. Ketogenic diet
Improves inflammation and insulin sensitivity. Not necessary for everyone, but may be helpful in some cases.
3. Low-meat diet
Reduces intake of leucine and other amino acids that activate mTORC1.
4. Antioxidant-rich diet
Neutralises free radicals and reduces inflammation, which is key in acne.
Conclusion
Although acne is multifactorial, we now know that diet does influence its development and progression. Reducing the glycaemic index of the diet, limiting unfermented dairy products, balancing fat consumption, increasing antioxidants and improving the microbiota can make a real difference to the skin.
Therefore, personalised nutritional intervention is an excellent complement to conventional dermatological treatment, allowing the hormonal, metabolic and inflammatory root causes of acne to be addressed.